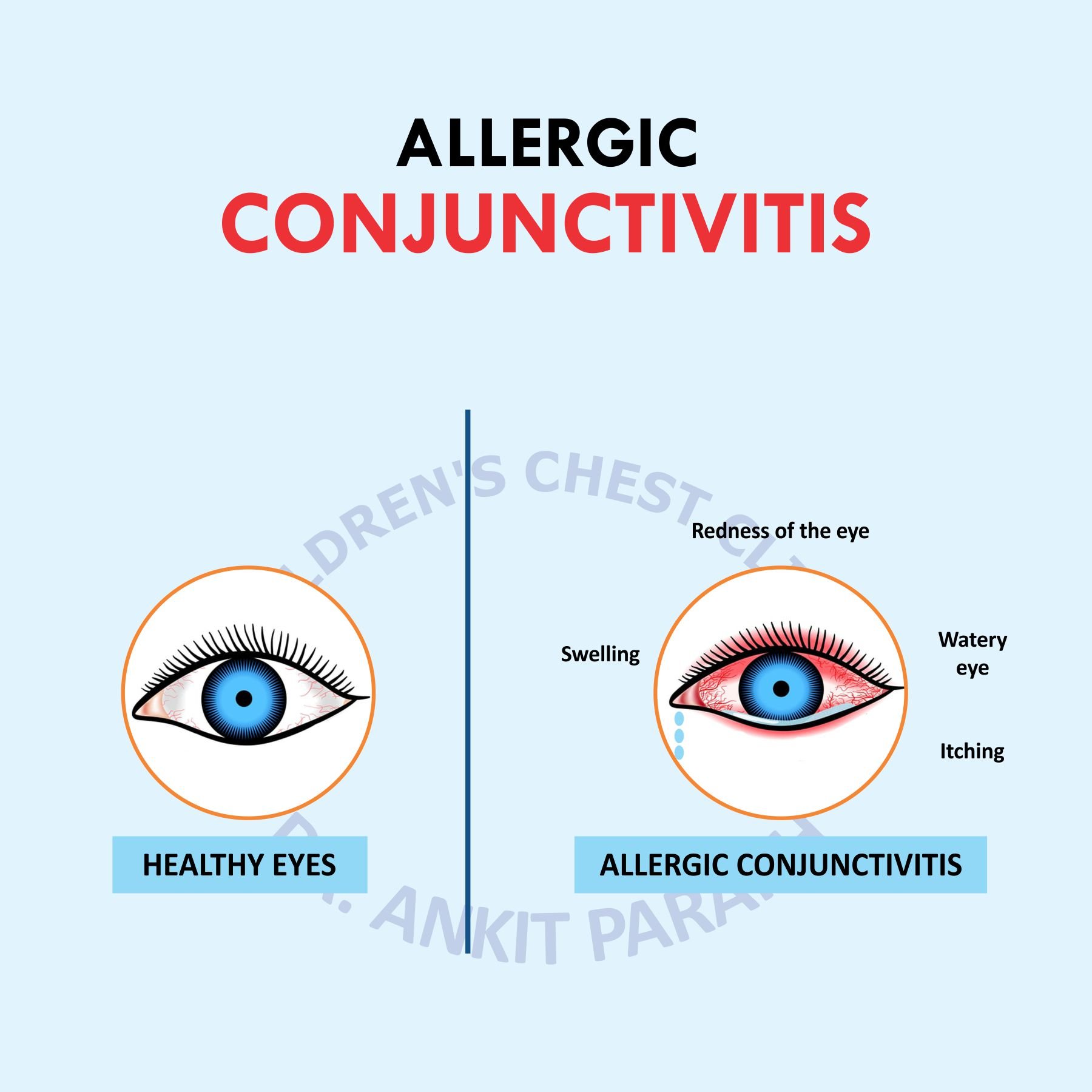
Allergic conjunctivitis is an inflammatory response of the conjunctiva to an allergen. Patients typically present with redness and swelling of the conjunctiva (the white visible part of the eye) with severe itching and increased watering sometimes associated with rhinitis (Running nose)
Allergic conjunctivitis can be Seasonal or Perennial. Seasonal Allergic Conjunctivitis has a more rapid presentation, typically after airborne exposure to pollens. Perennial Allergic Conjunctivitis has a milder presentation that can last year-round, triggered by various allergens
Common triggers for allergic conjunctivitis include household dust, pollen, mold spores, pet dander, household detergents, and perfumes. Pollen is a common cause of seasonal allergies, but a persistent allergy may be due to dust or animal dander, allergens that are present all year
Diagnosis is mostly clinical and blood test for allergic conjunctivitis is of not of much use and better avoided
DO’s and DON’Ts to prevents Allergic Conjunctivitis
- use only scent-free soaps and detergents
- install an air purifier in your home
- vacuum and dust regularly. Eyewash is a must after sweeping and dusting
- limit the carpets, soft toys, curtains, and soft furnishings in your home
- Use protective sunglasses while going outside
- Avoid handling flowers
How to treat Allergic Conjunctivitis
Household remedies like cold compression and artificial tears can reduce your symptoms to some extent. In severe cases consult your eye specialist. Your doctor may give you some anti-allergic or anti- inflammatory eye drops or low potential steroid eye drops in tapering doses. Never put steroid without doctor consultation. It may give you rapid relief but can cause cataract and glaucoma in long term use.
Severe allergies should be treated aggressively because chronic allergy can aggravate some eye diseases like Keratoconus and Limbal stem cell deficiency.